This year has been heavy. In March, we lost my mother-in-law. In June, my mom passed away. Out of four parents, only my dad remains, and he’s not in the best of health.
At age 68, my dad was diagnosed with heart failure. Just weeks ago, he was hospitalized for fluid buildup that had spread everywhere: around his lungs, his heart, his legs, his stomach. His condition is not something you “fix,” but it is something you can manage if you have the right care.
Encouraging, right? Unfortunately, after receiving that glimmer of hope, things started to unravel.
A Hospital Discharge Without a Plan
On August 30, the hospital discharged my dad. The process should have been straightforward. Instead, it was chaotic and careless.
- Timing. He was told he’d be released a day earlier than planned, with paperwork and prescriptions delayed until the evening.
- Medication. We weren’t made aware of what he needed until after 5:30 p.m., when most pharmacies were already closing. The medication wasn’t optional; it was critical for his health and safety after discharge.
- Support. When I asked about a starter dose to get him through the night, I was told “policy” wouldn’t allow it. A supervisor confirmed the same.
So there I was, faced with the choice of racing to a late-night pharmacy located an hour away and then driving another hour to my dad’s house or leaving him without the medicine needed to keep him stable. When I raised this concern with his nurse, her response was dismissive, suggesting I could simply bring the medication to him in the morning. That showed a lack of understanding of the practical realities of caregiving.
I asked to speak to a supervisor, who also confirmed the policy. When I pressed for clarification on why prescriptions had not been handled earlier in the day, she became defensive. Instead of offering to help—she called security.
Escalation to Security
Within moments, two officers arrived and stood watch over us. Then came a loudspeaker announcement across the hospital: “Avoid Room 512. Clear the area.”
We hadn’t raised our voices. We hadn’t made threats. We were asking why prescriptions had been left until the last minute. Yet we were treated like we posed a threat.
That’s what still stings. In a moment when we needed caring and collaboration, we were branded as a problem.
As of writing this, I haven’t heard back from the hospital about the formal complaint letter I filed on September 2. And if I’m honest, I don’t expect to.
A Familiar Story
The whole experience left me with a sense of déjà vu. I couldn’t help but remember my mom’s years of struggle with mental illness and the way hospitals often treated her.
One hospital discharged her in the middle of the night and sent her home in an Uber. There were the failed attempts at securing a 302, involuntary treatment during a crisis, even though it was clear she was a danger to herself and others.
And then there was the time she wound up in a homeless shelter because the hospital “didn’t want to deal with it.”
Different circumstances, same pattern. Policies and liability fears too often trump compassion and common sense.
The Good Stuff
It was a challenge for me to make sure Dad had all of his needs taken care of once he got back home, especially because of the distance. Fortunately, there were people who stepped in to help.
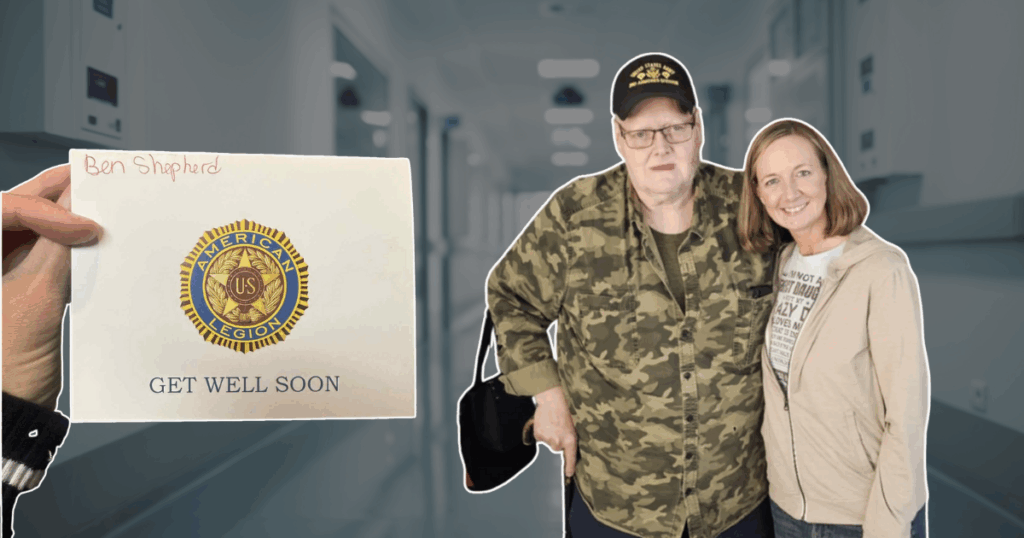
Neighbors and friends coordinated meals so he didn’t have to worry about cooking. The cleaning lady I hire twice a week took on extra errands, picking up groceries when he couldn’t. Friends and family checked in, and made sure he knew he wasn’t forgotten. Even simple gestures, like cards passed around at the VFW and American Legion, reminded him that people were thinking of him.
Those efforts may seem small, but to us they meant everything. They lifted some of the weight off my shoulders and gave my dad a sense of connection during a very isolating time.
What’s Next
Dad is keeping up with his medication and follow-up appointments, but where he lives is far from his providers and he’s on his own. My townhome isn’t suitable either, since there’s no first-floor living space.
What he needs most is to be closer—closer to me and closer to doctors and specialists who can monitor his condition without every appointment turning into an exhausting drive. That’s what I’m working toward now, finding a place where Dad can live with us, where distance and isolation are no longer part of the equation.
Final Word
Hospitals will say their policies are in place for safety. But when policies override people, it’s families like mine that carry the burden.
Still, in the midst of the frustration, I’m reminded of something important: while systems can fail us, people often don’t. Friends, neighbors, coworkers—their kindness has been the thread holding everything together.
That’s true outside of health care, too. In leadership, business, and even social media, policies and processes have their place. But when they become more important than people, we lose trust. What lasts isn’t the checklist or the protocol. It’s how you make others feel, whether they’re a client, a team member, or a loved one.
For that reason, I’ll continue to advocate for my dad, and I’ll continue to build my work the same way. Because in the end, people remember the compassion, the connection, and the support.
For that, I am thankful.