I turned 43 this past week, and I’m grateful for another trip around the sun and more adventures in life! With the passing years comes a familiar rite of passage: heightened medical screenings. In my case, it's the inevitable yet dreaded mammogram.
As you may know, breast cancer screening recommendations call for women to get annual (or, if you go by the most recent guidelines, biennial) mammograms beginning at age 40. However, exceptions may apply for those with a family history of breast cancer or individuals experiencing symptoms or abnormalities warranting earlier screenings.
At 41, I underwent my first screening, relieved to emerge without any concerns. So, you can imagine my shock when, at 42, I faced the dreaded “callback.”
The call came, requesting further imaging. The woman who called explained the presence of breast asymmetry — an area of increased density in one breast when compared to the corresponding area in the opposite breast.
I knew I had dense breasts, but I couldn't understand why one looked different, especially since my scans from last year were clear. The woman explained that their office didn't have the proper technology to address this issue, and she advised me to call and schedule a diagnostic mammogram, with ultrasound, if necessary, at a local imaging provider. She gave me the proper medical codes and information to arrange the appointment.
Enter Dr. Google.
Naturally, I panicked. And that’s when I went to Google for answers. If you’ve listened to my podcast, you know that my co-host and I call these exploratory online searches “Dr. Google.”
I stumbled upon various credible sources, but one from Medical News Today caught my attention. It stated that according to a study from 2021, “Women with asymmetrical breast density have an increased risk of developing breast cancer. In fact, their lifetime risk of developing the disease is four to six times higher compared with women of the same age with low breast density.”
This news understandably triggered more fear.
However, what I didn't grasp at the time was that although my breast tissue appeared asymmetrical in the scan, it didn't necessarily indicate a problem. This emphasizes the importance of additional imaging because such discrepancies are often due to healthy breast tissue overlapping. Unfortunately, my initial Google search sent me spiraling into fear. I spent time in endless online searches, stumbling upon statistics that only heightened my anxiety.
My advice to anyone undergoing further imaging due to a callback is simple: Don't panic. And try to avoid Google!
Why Density Matters
Let’s talk about breast density for a moment. For reference, breast density refers to the amount of glandular and connective tissue compared to fat tissue in the breasts as seen on a mammogram.
Generally speaking, as women age, their breast density tends to decrease. However, individual variations exist, and some women may maintain higher breast density, which is a risk factor for breast cancer because it can make it harder to detect abnormalities on mammograms.
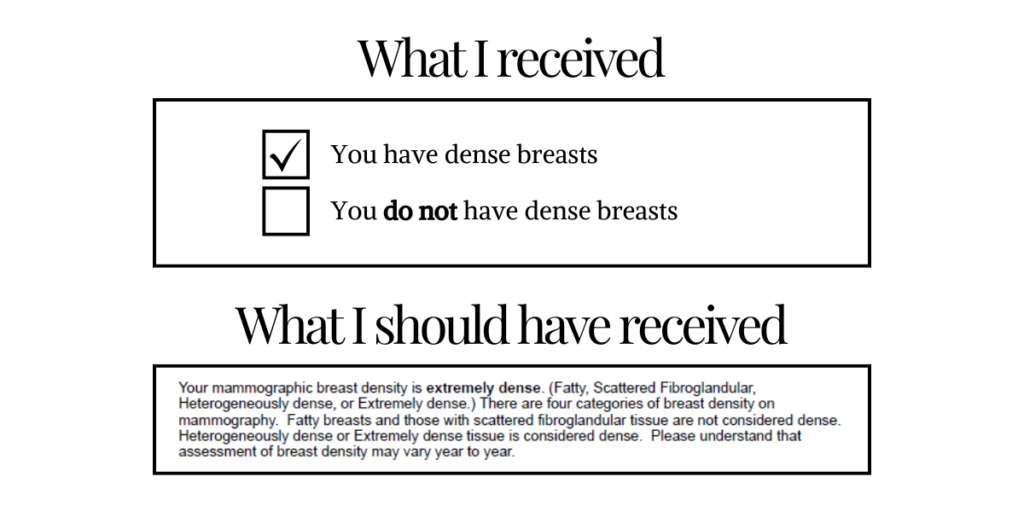
When I received the scans from my initial mammograms at ages 41 and 42, the information provided was limited to a simple checkbox indicating whether or not I had dense breasts. It wasn’t until later that I discovered every woman has a breast density grade, designated as A, B, C, or D. Understanding this grading system is crucial for women to make informed decisions about their screening routines and interpret the results.
After the diagnostic scans, I learned that I fell into the D category, a classification shared by around 10% of women. Additionally, I discovered that between 40% to 50% of women are categorized as either C or D, indicating a significant portion of the population has dense breasts. However, without further context, it's challenging to grasp the implications of this information and how it influences our screening processes.
If you're among the 10% of women with extremely dense breast tissue on mammograms, like me, you would benefit from a discussion of additional screening options like ultrasound or breast MRI with your doctor. Even if your breast density isn't in the extreme category, it's still worth considering extra testing and discussing your breast cancer risk assessment with your healthcare provider. Dr. Jennifer Harvey from the University of Rochester Medical Center emphasizes that supplemental screening can be beneficial for those with dense breasts, as mammography alone may not be sufficient for early breast cancer detection.
Remember, higher breast density can both mask cancer on a mammogram and increase the risk of developing breast cancer, so you have a right to this information. In fact, providers have until September 2024 to implement and abide by the rule added to the Mammography Quality Standards Act (MQSA) of 1992. The addition mandates that providers include an assessment of a patient’s breast density in a mammogram report to inform them about the potential limitations of their screening and enable them to make an informed decision about further testing with their doctor.
“In extremely dense breasts, a mammogram will miss cancer almost half the time, and they’re four to six times at greater risk of getting breast cancer than those with the least density,” said JoAnn Pushkin, executive director of DenseBreast-Info.
There’s that statistic again, but if you review that against the earlier quote in the opening of this post (under Enter Dr. Google), you’ll notice one difference. In the earlier quote, it reads, “Women with asymmetrical breast density have an increased risk of developing breast cancer…” and in this quote, it reads, “In extremely dense breasts….”
So, which is it: asymmetrical or extreme density? Or are both true? I have yet to figure out the correct answer, but one thing is for certain: increased density means increased risk. And mammograms do not adequately detect cancer in higher-density breasts.
My advice to anyone attending a routine mammogram screening: Ensure you receive your density results and request your density grade!
Why Aren’t Routine Mammograms Detecting Common Issues?
As I awaited my diagnostic scan results, I asked why initial mammograms don't always detect issues, especially considering nearly 50% of women have dense breasts.
I was told that most places have a 3D machine, which is what they used during my follow-up mammogram. As far as she was aware, the place where I received my initial screening only had a 2D machine. After I left, I went to the website of my mammography place only to find that they do have a 3D machine…So what was I missing?
Time to investigate.
I contacted the folks who conducted my initial mammogram screening and spoke to their mammographer. She confirmed they have the 3D technology and explained how they capture the four images — with two scans of each breast in different positions.
She also explained that while many places have 3D technology, not all have on-site radiologists to interpret the scans immediately. At places like UMPC, for instance, radiologists can read the scans promptly and recommend further testing if needed, which is why the ultrasound, if necessary, was scheduled directly after the diagnostic mammogram.
My question still stands: Why aren't initial mammogram screenings capable of proper scanning for unhealthy breast tissue, especially considering that the callback screening cost is several hundred dollars?
My advice to anyone who has a callback: Continue to ask this question!
Is Mammography The Best Way to Screen?
There’s been some controversy regarding mammography. Switzerland has banned mammograms, citing concerns over false positives and the potential harm outweighing the benefits as primary reasons. However, they do promote ultrasounds and MRIs as alternatives.
A TIME article shed further light on the mammogram debate. According to their large-scale review, “The findings are that breast cancer is over-diagnosed, with small growths that likely aren’t going to progress into cancer being detected — and treated — more than they need to be. Meanwhile, the truly dangerous tumors, which develop into advanced cancer that spreads to other parts of the body, are being missed.”
Well, that’s scary. And it negates the point, right? Well, not necessarily.
There are people who share that early detection has been key to their survival, and many will argue that mammograms detected the initial mass. This was the case for the mother of someone on the #Strella team when she was diagnosed with breast cancer at age 59. She underwent a year-long process of chemo, surgery, and radiation — and she successfully responded to the treatment.
So, screening is valuable for many women. However, I question if mammography is the best way to screen. With so many women with high-density breasts and nearly half of cancers going undetected by mammograms, why would this method be the standard?
More questions arise…
- Is this a way to make money since the costs start to incur when additional scans are needed?
- Should we be lobbying for insurance to cover a better initial detection system — for all women?
- What do we have to do to make this process less invasive, less stressful, and more comfortable?
- What do we have to do to make these results more accurate?
These are all questions that may be going through your head, as well.
My advice to anyone who has a callback: Do not stop asking these questions! And, as you make progress, leave a comment on this post so we can continue to help other women find answers.
What My Results Revealed
All this said, you’re probably wondering what happened with my scans. Well, I was relieved to find that the diagnostic mammogram showed no signs of cancer, and I was free to go without an ultrasound or any further testing. The technician explained that it was breast tissue that folded over itself, which is common with dense breasts.
Well, thank you, God!
Considering the statistics, whatever they may be, can I confidently say I'm out of the woods? Will this cycle just repeat again?
It's evident that our current system isn't effective, resulting in numerous women undergoing extra tests, enduring unnecessary stress, and bearing additional financial strain. I urge you to inquire further! Together, we can seek solutions that lead to improvements that save time, money, and lives.
My final word advice to anyone who receives a callback: It will be OK.